Sunday, December 13, 2015
Synovial fluid replacement therapy
Labels:
arthritis,
arthroscopy,
best orthopedic doctor,
knee injection,
knee joint,
knee pain,
orthopedic clinic,
orthopedic doctor ameerpet,
orthopedic doctor apollo hospital,
osteoarthritis
Sunday, November 22, 2015
HEEL AND FOOT PAIN
HEEL & FOOT PAIN
Heel pain is an extremely common complaint, and there
are several common causes.
 Plantar Fasciitis: It is the most common condition that causes heel pain.
Plantar fasciitis is due to irritation and inflammation of the tight tissue
that forms the arch of the foot. The most common symptom is pain under the heel
after a period of rest, i.e. severe pain and inability to walk in the morning
after getting up from sleep. The same might happen after sitting for a long
time and then trying to walk. Interestingly the pain gets better after a few
steps though it may not go away completely.
Again, the pain may get worse with prolonged walking and standing. X ray
may show a bony spur which may develop in long standing cases of heel pain due
to plantar fasciitis, but it may not cause the symptoms.
Plantar Fasciitis: It is the most common condition that causes heel pain.
Plantar fasciitis is due to irritation and inflammation of the tight tissue
that forms the arch of the foot. The most common symptom is pain under the heel
after a period of rest, i.e. severe pain and inability to walk in the morning
after getting up from sleep. The same might happen after sitting for a long
time and then trying to walk. Interestingly the pain gets better after a few
steps though it may not go away completely.
Again, the pain may get worse with prolonged walking and standing. X ray
may show a bony spur which may develop in long standing cases of heel pain due
to plantar fasciitis, but it may not cause the symptoms.
Posterior Heel Pain: Posterior heel pain causes symptoms behind the foot,
rather than underneath. Posterior heel pain causes include Achilles tendinitis
and retrocalcaneal bursitis. These patients may also develop bony growth behind
the heel bone and when they are large may lead to rupture of Achilles tendon.
Patients may have difficulty to walk comfortably on the affected side and pain
that occurs at night or while resting.
Treatment Options:
Not all of these treatments are appropriate for every
condition, but they may be helpful in your situation.
1.Rest - Avoiding the precipitating activity; for
example, take a few day off jogging or prolonged standing/walking. Rest can reduce the severity of pain and will
allow the inflammation to begin to cool down.
2.Ice Packs
- Icing will help to
diminish some of the symptoms and control the heel pain. Icing is especially
helpful after an acute exacerbation of symptoms.
3.Exercises and Stretches
- Are designed to relax
the tissues that surround the heel bone. Some simple exercises performed in the
morning and evening, often help patients feel better quickly.
4.Anti-Inflammatory Medications
- Help to both control
heel pain and decrease inflammation.
5.Shoe Inserts
- Are often the key to
successful treatment of heel pain. The shoe inserts often permit patients to
continue their routine activities without heel pain.
6.Injection
therapy - In
some cases, corticosteroid injections are used to help reduce the inflammation and
relieve pain.
7.Removable
walking cast - May
be used to keep your foot immobile for a few weeks to allow it to rest and heal
and is used only for severe cases.
8.Night splint
- Wearing a night splint
allows you to maintain an extended stretch of the plantar fascia while
sleeping. This may help reduce the morning pain experienced by some patients.
9.Weight
reduction – It helps to reduce stress on foot and heel and
thus help to reduce the severity of pain.
If, after several
months of non-surgical treatment, you continue to have heel pain, surgery will
be considered.
Healthy Joint
Club says:
Not being able to take first step out of bed in the
morning can be frightening. More over severe pain from the heel may force you
to restrict several day time activities. Except for a handful of cases and some
uncommon conditions, most cases improve with treatment and time. Even though
the time taken for the recovery may vary from person to person there is a
natural tendency for these conditions to get better spontaneously.
STRETCHING
EXERCISES
1.PLANTAR FASCIA STRETCH:
Sit in a chair and
cross one foot over your other knee. Grab the base of your toes and pull them
back toward your leg until you feel a comfortable stretch. Hold for 10 seconds
and repeat 5 to 10 times.
2.ACHILLES STRETCH:
Stand on forefoot
at the edge of stair, reach the step below with your heel, until you feel the
stretch in the arch of the foot. Hold this position for 10 seconds and repeat 5
to 10 times.
3.HEEL RAISE:
Stand behind the
chair or any support and raise your body up onto your toes and hold for 5
seconds. Then slowly lower down yourself. Repeat 5 to 10 times.
4.TOWEL PICK:
Drop a towel on the
ground and pick up the towel with your toes. Release and repeat 5 to 10 times.
5.FROZEN CAN ROLL:
Take a frozen
juice can or tin, roll your feet on the can from front to back. Do it for 3 to
5 minutes.
6.TOWEL STRETCH:
Loop a towel
around your toes and pull the foot towards your body keeping your leg straight.
Hold this for 10 seconds and relax. Repeat 5 to 10 times.
Dr.A.Mohan Krishna
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
Labels:
apollo hospital,
best orthopedic doctor,
calcaneal spur,
foot pain,
gout,
heel pain,
heel spur,
orthopedic doctor ameerpet,
orthopedic doctor apollo hospital,
orthopedic hospital,
plantar fasciitis
TAIL BONE PAIN - COCCYDYNIA
Pain in the tail bone can frustrate, irritate and
embrace many patients for getting the treatment. This condition can be curable
and prevented if proper care is taken.

Any irritation
(inflammation) of the bony area (tail bone) situated between the folds of the
buttocks is referred as Coccydynia.
The usual
complaint is pain at the bottom region of the back on sitting. It is usually
caused by injury, during pregnancy, chronic pressure on the tail bone due to
sitting for long hours as of in those involved in driving occupation. Sometimes
tail bone pain occurs in patients with chronic constipation. In one third of
the cases the cause is not known.
Coccydynia is
usually diagnosed based on the typical complaints and sometimes by an x-ray.
Clinician can diagnose by examination and eliciting tenderness at the local
region. It is necessary to directly visualize the tailbone region to rule out
other causes and any infection. Sometimes infection of the hair follicles at
the tailbone region can mimic coccydynia.
This
condition usually frustrate patients and impair the quality of life. Sometimes patients feel embarrassed to get
the treatment.
Treatment is usually by activity modification, anti inflammatory medications
and local injections. Surgery is rarely indicated in non responsive cases. Since long hours
of sitting may aggravate the condition, a modified padded cushion with cut out
at the back could relieve the pressure on the coccyx. (Doughnut cushion).
Pelvic floor exercises could help to get relief from pain. Use of stool
softeners and laxatives in cases of constipated patients could help to relive
pain. Seitz bath by sitting in tub of hot water may provide pain relief.
Since long hours
of sitting may aggravate the condition, a modified padded cushion with cut out
at the back could relieve the pressure on the coccyx. (Doughnut cushion).
Pelvic floor exercises could help to get relief from pain. Use of stool
softeners and laxatives in cases of constipated patients could help to relive
pain. Seitz bath by sitting in tub of hot water may provide pain relief.
Oral anti
inflammatory medications and local application of pain gels may tries to relive
the symptoms. Local trigger injections with low dose steroid preparations will
aid in complete relief in majority of cases. These local injections can be
given by the doctor in the outpatient department. In rare case surgical treatment by removal of
coccyx may be required in those cases not responding to conservative methods.
Dr.A.Mohan Krishna
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
BACK PAIN IN PREGENACY
BACK PAIN IN PREGNANCY
Back pain is the most common orthopedic
complaint in most of the pregnant women. According to the scientific literature
50% to 80% of the pregnant women complain of back pain at sometime during their
pregnancy. Out of the different back pains it is the lower back pain which most
of the pregnant mothers suffer.
Number of factors can be attributed for
the cause of low back pain in the pregnancy. Hormonal and postural changes play
a major role in the cause.
During pregnancy many hormones are
produced out of which Relaxin is the one which is of our concern. The function
of hormone Relaxin is to loosen the joints and ligaments in your body. This
helps to relax the ligaments in the pelvis which in turn makes room for your
baby inside and also helps during delivery of your baby.
Since the hormone have no selective role
in relaxing the ligaments and joints of the pelvis only, all the ligaments and
joints in the body are stretched. Laxity of the ligaments which support the
spine results in the instability which can cause back pain.
As the baby grows and size of the uterus
expands, the posture of your body is altered resulting in forward bending of
lower spine and compensatory backward bending of upper spine. Abdomen shifts
forwards and downwards altering the normal biomechanics of the spine. This in
turn adds on strain to back muscles which may become sore and tired.
Two types of lower back pain are
observed during pregnancy,
- Lumbar
pain
- Posterior
pelvic pain
Lumbar pain
It is similar to the kind of back pain
that you may have experienced before the pregnancy. It is caused by sitting or
standing for prolonged periods. It presents as pain in the lower back, just
slightly above the waist line.
Posterior pelvic pain
It is the pain experienced at the back
of the pelvis, below the waist line, across the buttocks and near the tail
bone. It is the most common type experienced by pregnant women. It can be
aggravated by bending twisting, climbing stairs, or leaning forwards.
Management
Back pain during pregnancy could be
controlled and prevented by taking necessary precautions and following regular
exercise protocol. Exercises help to strengthen, stretch the back muscle. These
include pelvic tilt exercises, back stretches, hamstring stretches and kegel exercises.
Walking and swimming are the two
preferred exercises during pregnancy to maintain the tone of back muscles.
Walking helps to maintain flexibility of muscles of lower back, hips and knee.
Swimming and other aquatic exercises allows full body work out with minimal
stress and strain to the body. Prenatal yoga or pregnancy yoga helps to stretch
and strengthen the back muscles and aid in relieving the pain.
It is not only exercises which help in
controlling the back pain, but maintaining proper posture while standing and
sitting will help. When you stand try to tuck your hips and pelvis, try resting
one foot on a stool. Prolonged sitting can hurt you back, so take frequent
breaks if you plan to sit for long times. Safe lifting and bending practices help
you to prevent undue strain on your back. When bending over to lift any object,
bend at the knees instead at waist and use your thigh muscles to push yourself
up instead of back muscles. Try not to lift heavy objects. Wearing low heeled
shoes with good arch support may help to alleviate back pain.
Sleeping posture most favorable for
pregnant women is to sleep sideways, preferably on left side. Try sleeping with
your knees and hip bent, with pillows between knees and one under the belly.
Note:
If you are pregnant with sever back
pain, which is rhythmic and feels like menstrual cramps consult your doctor. If
you have back pain with numbness or weakness in both lower limbs it needs
urgent evaluation by your doctor. Dull back pain during late stages of pregnancy
could be signs of preterm labor.
Dr.A.Mohan Krishna
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
Labels:
apollo hospital,
back pain,
back problems,
orthopedic doctor,
orthopedic doctor ameerpet,
orthopedic doctor apollo hospital,
orthopedic hospital,
pain in back,
pregnancy,
spine
Thursday, November 19, 2015
Arthroscopy (keyhole surgery)
What is Arthroscopy?
Greek word for joints is “Arthros”, and
Greek word for looking is “Scope”, so arthroscopy means looking in to the
joints. Since this is done through a small cut it is commonly known as a
minimally invasive surgery or a key hole surgery. It can be performed on many
joints like shoulder, elbow, wrist, hip, knee and ankle joints, though shoulder
and knee are the commonest.
Why Arthroscopy?
When investigating the conditions of the
joints it is very helpful to be able to
look inside the joint in order to see exactly what is going on in addition to
examining the joint from outside. It is done with special equipment. Operative
procedures for any abnormalities can be done through a second small cut. It is
routinely done as a planned procedure as a day case, but sometimes it is done
as a matter of urgency, for example following injury to a joint like a twisted
swollen knee joint.
What are the advantages?
a) Small incisions and small scares.
b) Less tissue damage and less chance of
infection.
 c) Less pain and disability after surgery
and patient can return to sedentary work almost immediately and to more
vigorous work within 1 to 2 weeks.
c) Less pain and disability after surgery
and patient can return to sedentary work almost immediately and to more
vigorous work within 1 to 2 weeks.
d) Better diagnosis of many joint problems.
e) Most procedures can be performed as outpatient
basis. If hospitalization is required most procedures need 1-2 days of stay
compared to several days of stay with open procedures.
f) Some procedures can be done better with
arthroscopic surgery and perhaps for some that is the only way they can be
done.
Preparation for surgery
 After deciding to proceed with arthroscopy
some basic blood tests are done and patient’s fitness is assessed. Like any
other surgery patients would be asked not to eat or drink any for at least 6
hours prior to surgery. Patients can watch the surgery if it is done under
regional anaesthesia.
After deciding to proceed with arthroscopy
some basic blood tests are done and patient’s fitness is assessed. Like any
other surgery patients would be asked not to eat or drink any for at least 6
hours prior to surgery. Patients can watch the surgery if it is done under
regional anaesthesia. After surgery
Prescription would be given for pain killer
tablets and other medicines as necessary. The joint needs to be rested a little
for a couple of days but like in case of arthroscopy of the knee joint you can
walk to and from the toilet with crutches but to avoid excessive use of the
joint. One important aspect is physiotherapy to get full movement in the joint
and to strengthen the muscles around the joints. Within the limits of pain
these exercises can be started as soon as possible after surgery. The exercises
can be carried out many times in a day.
Start with 4-6 repetitions of each exercise, increasing to as many as
you feel able to do without getting any pain. When you had any other
reconstructive surgery like ligament and meniscal surgery post operative care
and advice will be different. Similarly arthroscopy of shoulder would be
followed up by specific exercises depending upon the type surgery. You would be
asked to visit the hospital after 2 days for a change of dressing.
Common conditions needing Arthroscopy
Knee Arthroscopy:
 A torn meniscus ( to repair or remove), a
torn anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL), For
removal or biopsy of inflamed or damaged lining of the joint(synovium),
Misalignment of the kneecap (patella), Small pieces of broken cartilage and
loose bodies in the knee joint, Removal of Baker's cyst(a swelling behind the
knee that is filled with fluid), Some fractures of the bones of the knee.
Washing the knee which is constantly sore due to arthritis can also be
beneficial.
A torn meniscus ( to repair or remove), a
torn anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL), For
removal or biopsy of inflamed or damaged lining of the joint(synovium),
Misalignment of the kneecap (patella), Small pieces of broken cartilage and
loose bodies in the knee joint, Removal of Baker's cyst(a swelling behind the
knee that is filled with fluid), Some fractures of the bones of the knee.
Washing the knee which is constantly sore due to arthritis can also be
beneficial.Shoulder Arthroscopy:
 Arthroscopy of the shoulder may be
recommended for infective arthritis(septic lesions), biceps tear, SLAP lesions,
Rotator cuff lesions, impingement syndrome, recurrent dislocation of shoulder
and other instability problems with or
without hyper laxity, Frozen shoulder, loose bodies etc. Problems associated
with the other joints in shoulder joint complex i.e. subacromial joint,
acromio-clavicular joint are also easily examined giving access to rotator cuff
lesions, acromion pathology and clavicular
problems.
Arthroscopy of the shoulder may be
recommended for infective arthritis(septic lesions), biceps tear, SLAP lesions,
Rotator cuff lesions, impingement syndrome, recurrent dislocation of shoulder
and other instability problems with or
without hyper laxity, Frozen shoulder, loose bodies etc. Problems associated
with the other joints in shoulder joint complex i.e. subacromial joint,
acromio-clavicular joint are also easily examined giving access to rotator cuff
lesions, acromion pathology and clavicular
problems.Thursday, November 5, 2015
AVASCULAR NECROSIS OF FEMORAL HEAD
Bone is a living tissue and it needs blood supply to survive. If
there is damage to one of the blood supply, bone may depend on the accessory
blood supply for the survival. But certain bones in our body have precarious
unidirectional blood supply like Head of femur, scaphoid, and talus.
When there is damage to blood supply to the head of femur it
results in the death of cells in the femoral head. Gradually there is collapse
of femoral head with loss of sphericity. This condition is referred to as
Avascular necrosis of femoral head or Osteonecrosis (bone death) of femoral
head.
How AVN develops in femoral head?
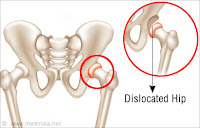
Hip joint is a ball and socket type of synovial joint. The socket
is formed by cup shaped acetabulum which surrounds the ball (femoral head -
upper end of thigh bone). The surface of femoral head and socket is lined by
thick articular cartilage and then lined by synovial membrane. All together
with the surrounding joint capsule and muscles form a hip joint.
The ball of hip joint receives most of its blood supply through
the neck of thigh bone. If there is damage to this blood supply there is no
accessory blood supply to the femoral head.
There is gradual death of cells in femoral head due to loss of
blood supply. Due to death of bone cells, there is no reparative process of
bone formation and resorption. Gradually the bony structure in the femoral head
weakens and starts to collapse. When AVN develops in the head femur, the weight
bearing area of the head is the first place to collapse. The rounded contour of
the femoral head is lost and it becomes flattened causing abnormal movement in
the hip joint.
Secondary osteoarthritis develops, as there is gradual wear in
ball and socket of the hip joint.
Causes:
Many causes have been identified
Trauma:
Fractures
Damage to the blood supply of femoral head usually occurs following a trauma or fractures to the bones in and around the hip joint.
Ø Fracture of Femoral neck, Femoral head
Ø Hip Dislocations
Ø Bad fractures of acetabulum
AVN can develop months or some times after initial injury.
Drugs:
Steroids:
Some steroids like cortisone,
prednislone or methyprednisolone are known to cause AVN. In certain conditions like bronchial asthma,
skin diseases, some auto immune disorders, inflammatory arthritis and in cases
of organ transplant to prevent rejection, use of steroids is must to control or
treat these conditions. Orally prescribed steroid are notorious in producing
AVN of femoral head. There have been studies to show that steroid given in the
form of injections into the joints or bursa does not cause any AVN of femoral
head.
Blood
disorders:
Some blood diseases like sickle cell disease, Leukemia’s, Gauchers
disease and diseases related to blood coagulation can cause AVN of femoral
head.
Lifestyle:
Studies have shown that alcohol and smoking can cause AVN in
femoral head. Chronic alcohol intake can damage blood vessels leading to AVN.
Smoking cause narrowing of small blood vessels and thereby reducing blood
supply to the femoral head.
Others:
Deep see divers and miners are more prone develop AVN. Due to high
atomospheric pressure tiny air bubbles are formed inside the blood stream which
can block the tiny blood vessels in the femoral head there by resulting in AVN.
Symptoms
What
does AVN feel like?
1. Pain:
Initially
patient complains of pain in the affected hip which gradually increases on
weight bearing. As the disease progresses patient complains of pain at rest and
at night.
2. Limping
3 3.Stiffness
4. Difficulty in sitting cross legged and squatting
5. Shortening of affected limb
Diagnosis
How do doctors identify the condition?
History: doctor inquires
about
- Occupation
-
Medical problems and any medications like steroids
-
Alcohol and smoking
2 Examination: doctor examines
hip for
- Range
of movements
-
Stiffness
X-rays:
X - rays do not show any changes of AVN in the early stages of disease even though patient is having pain in the hip. It may take few months to observe changes of AVN and make diagnosis on X - ray.
X - rays do not show any changes of AVN in the early stages of disease even though patient is having pain in the hip. It may take few months to observe changes of AVN and make diagnosis on X - ray.
MRI:
MRI can detect early
changes of AVN in the femoral head that cannot be seen on X- ray. It helps to
detect damaged areas of blood supply to the hip. AVN of femoral head can be
graded as mild, moderate and severe depending on the size location of these
damaged areas and if any collapse has occurred in the MRI images. MRI can also
help to detect AVN changes in the opposite hip even though there are no
symptoms.
Bone scan:
Bone scan involves
injecting a radioactive chemical into the blood. Hours after injection a
special camera is used to take pictures of your skeleton. The picture shows
blank spot in the areas of femoral head which is devoid of blood supply. MRI
has replaced Bone scan in diagnosing the cases of AVN of femoral head.
Treatment
What
are the treatment options for AVN of femoral head?
AVN of femoral head is irreversible resulting in arthritic hip.
Some drugs and salvage procedures can help in delaying the progress of
disease. The choice of treatment depends
upon the stage of the disease. Some factors like age of the patient, general
health of patient and activity level also determines the treatment methods.
Nonoperative
treatment:
If avascular necrosis of femoral head is diagnosed in early
stages, some of following treatment methods can help in delaying the progress
1.
Protected weight bearing on
the affected limb with the help of crutches or walker can help reduce pain. The
idea behind it is, it permits healing and prevents further damage.
2. Exercises and stretches prevent stiffness in the hip and helps to
maintain range of motion.
3. Medications:
A. Bisphosphnates : This group of drugs help to reduce the risk of
femoral head collapse in patients with Avascular necrosis.
B. Blood thinners: They are given in view of improving blood
circulation to the femoral head.
C. Anti-inflammatory medications / simple analgesics to reduce pain.
The above mentioned treatment modalities may delay the progression
of disease, but not completely reverse the Avascular necrosis.
Surgical management:
Salvage procedures: Some surgical procedures can try to decrease
the pressure in femoral head and increase the blood supply. The main
prerequisite for such surgeries is that there should not be any collapse in the
femoral head. Many procedures have been designed to improve the blood supply of
femoral head. Your surgeon can choose
and suggest appropriate procedure.
Core decompression of femoral head:
The most common surgical procedure is to drill one or several
holes into the femoral neck and head trying to enter into areas of poor blood
supply. The idea behind this procedure is one that it creates a new path for
new blood vessels to grow into areas of poor blood supply and it relieves
pressure inside the femoral head. The other advantage of this procedure is that
there is pain relief secondary to relieving pressure in the femoral head.
Core decompression of femoral head can be supplemented with bone
grafting with or without stem cells injection
Core
Decompression and Bone grafting of femoral head:
 Following core decompression procedure bone graft is packed into
the dead part of femoral head and channel created in the femoral head and neck.
The bone graft can be taken from the patient or from the bone bank. The bone
graft is made into tiny pieces and packed into the channel created in the
femoral head and neck.
Following core decompression procedure bone graft is packed into
the dead part of femoral head and channel created in the femoral head and neck.
The bone graft can be taken from the patient or from the bone bank. The bone
graft is made into tiny pieces and packed into the channel created in the
femoral head and neck.
Stem
cells treatment:
Stem cells obtained from the patient body can be injected into the
channel created for core decompression of femoral head. Stem cells injection
can be done along with bone grafting also. There are studies showing that stem
cells help to stimulate new bone formation in the diseased areas of the femoral
head.
Postoperative rehabilitation after core decompression surgery:
This surgical procedure is done through a very small incision from
the side of thigh. Surgeon guides the drill into the femoral head with help of
intraoperative X - ray machine
(C-Arm). This procedure is usually done as outpatient procedure and patient can
go back to the house on the same day with help of crutches or walker.
Following core decompression surgery the drill holes in the
femoral neck and head may weaken the bone, making it susceptible to fracture.
So patients are advised to use crutches or walker to move around for six weeks.
After six weeks, patient patients are advised to put full weight on operated
leg and take advice of physiotherapist to regain hip range of motion and
strength.
Advantages
of core decompression surgery:
Core decompression of femoral head is NOT A DEFINITIVE procedure.
It is a salvage procedure to delay the process of Avascular necrosis probably
by increasing blood supply and also preventing further collapse.
After the core decompression procedure it is necessary to
continue, the medications explained above as they also help in delaying the
progress of disease.
Core decompression and Vascularized fibular grafting:
In the first step surgeons drills a hole
into the femoral neck and head. In the next step surgeon removes small part of
fibula (Thin bone by the side of shin bone in leg) along with its blood
vessels. This is referred as vascularized fibular graft because it has its own
blood supply. Fibular graft is inserted into the channel created in the neck
and head of the femur. Vascular surgeon attaches the blood vessels from the
fibula to one of the blood vessels in the hip. This procedure does two things
1. Fibular graft acts as structural support
preventing collapse of femoral head.
2. The newly connected blood vessels try to
increase blood supply to the femoral head.
This is a very complicated procedure and
needs special expertise. The success of the surgery depends on the viability of
newly created blood supply. It is rarely practiced nowadays.
TOTAL HIP REPLACEMENT:
The process of Avascular necrosis of
femoral head invariably ends in arthritic hip. In arthritic hip, joint surfaces
of femoral head and acetabulum becomes irregular with loss of motion in the
joint. The treatment choice is total hip replacement.
Total hip replacement is procedure in
which the surgeon replaces the damaged femoral head and damaged joint surface
of acetabulum (socket) with prosthetic components. Damaged femoral head is
removed and replaced with metallic stem and ball. Damaged cartilage of the
socket of hip joint is replaced with metal socket.
Prosthetic components:
Total Hip replacement can be either
cemented or uncemented.
Cemented Total hip replacement: In this procedure, cement is used for fixation of
the prosthetic components into the bone.
Uncemented Total Hip replacement: In this technique, the fixation of components is by
“pressfit” into the bone which allows bone to grow onto the components.
Prosthetic materials:
Total hip replacement has wide range of
designs and materials.
The stem component and socket components
in the total hip arthroplasty are invariably medical grade steel or titanium
alloys. There is choice of material selection for the prosthetic head and liner
of socket. Prosthetic heads can be metallic or ceramic. Socket liners are available
in plastic, metallic and ceramic materials.
Different combinations of metal heads
and liners can be made depending on needs of the patient.
Ceramic on plastic (Ceramic head /
Plastic liner)
Metal on metal (Metal head / Metal
liner)
Metal on ceramic (Metal head / ceramic
liner)
Ceramic on ceramic (Ceramic head /
Ceramic liner)
The decision to use cemented or
uncemented components and various combination of head and socket liners are
based on various factors such as age, bone quality and sometimes surgeons
choice.
RESURFACING ARTHROPLASTY:
In certain patients with limited damage to the
part of femoral head surgeon may consider resurfacing arthroplasty. In this
procedure surgeon replaces only damaged femoral head with metallic implant.
Dr.A.Mohan Krishna
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
Dr.A.Mohan Krishna
M.S.Ortho.,MCh orth (U.K)
Consultant Orthopedic surgeon,
Apollo Hospital
Appointments
Cell: 9247258989
9441184590
email: bonesandjointsclinic@gmail.com
online appointments:
www.drmohankrishna.com
www.bonesandjointsclinic.com
Labels:
apollo hospital,
AVN femoral head,
core decompression,
hip arthritis,
hip pain,
hip replacement,
hip surgery,
orthopedic doctor,
orthopedic doctor apollo hospital,
orthopedic hospital
Subscribe to:
Posts (Atom)